Glaucoma
What is Glaucoma?
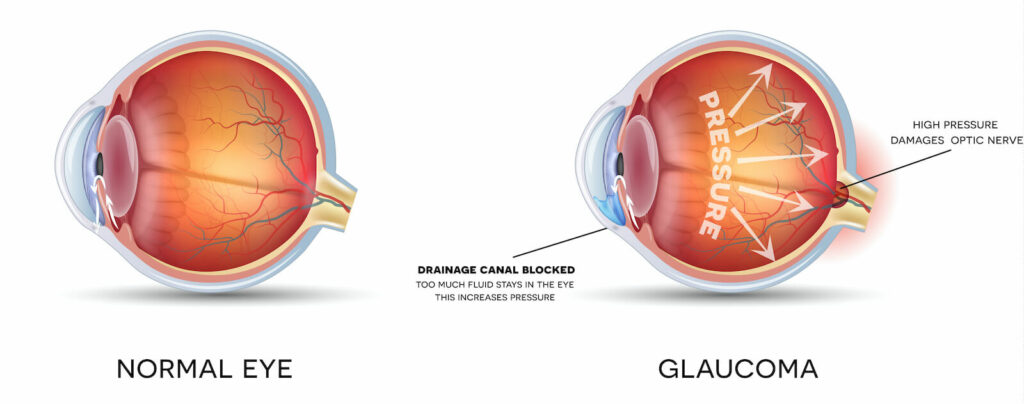
Glaucoma is the leading cause of blindness and visual impairment in the US, and can affect patients of all ages, many of who do not experience any symptoms and may not be aware that they have the disease. Glaucoma actually refers to a group of diseases that cause damage to the optic nerve as a result of increased pressure within the eye, but can also be caused by a severe eye infection, injury, blocked blood vessels or inflammatory conditions of the eye.
Many patients do not experience any symptoms during the early stages of glaucoma, including no pain and no vision loss. This makes it difficult for many patients to know if they have the disease. But as glaucoma progresses, patients may experience a loss of peripheral or side vision, along with sudden eye pain, headache, blurred vision or the appearance of halos around lights.
Glaucoma Symptoms
GEP – Glaucoma Symptoms. with Dr. Parul Khator from EyeSouth Partners on Vimeo.

Diagnosing Glaucoma
While some patients may experience symptoms from glaucoma as the disease progresses, others do not learn they have the condition until they undergo a routine eye exam. There are several different exams performed to diagnose glaucoma, including a visual field and visual acuity test. These tests measure peripheral vision and how well patients can see at various distances. Other tests may also be performed, such as tonometry to measure the pressure inside the eye and pachymetry to measure the thickness of the cornea.
Treatment For Glaucoma
Once glaucoma has been diagnosed, treatment should begin as soon as possible to help minimize the risk of permanent vision loss. There is no cure for glaucoma, so treatment focuses on relieving symptoms and preventing further damage from occurring. Most cases of glaucoma can be treated with eye drops, laser or microsurgery. The best treatment for your individual case depends on the type and severity of the disease, and can be discussed with your doctor.
- Eye drops are used to reduce fluid production in the front of the eye or to help drain excess fluid, but can lead to redness, stinging, irritation or blurry vision. Patients should tell their doctor about any allergies they have to minimize the risk of side effects.
- Laser surgery for glaucoma aims to increase the outflow of fluid from the eye or eliminate fluid blockages through laser trabeculoplasty, iridotomy or cyclophotocoagulation.
- Microsurgery involves a surgical procedure called a trabeculectomy, which creates a new channel to drain fluid from the eye and reduce the pressure that causes glaucoma. Surgery is often performed after medication and laser procedures have failed.
Preventing Glaucoma
While there are no surefire ways to prevent glaucoma from developing, regular screenings and early detection are the best forms of protection against the harmful damage that the disease can cause. While anyone can develop glaucoma, some people are at a higher risk for developing this disease. These people may include those who:
- Are over the age of 60
- African Americans over the age of 40
- Have a family history of glaucoma
- Have poor vision
- Have diabetes
Patients should have a comprehensive dilated eye exam at least once every two years, especially if they have a higher risk of developing glaucoma. Older patients may be encouraged to be tested more frequently.
To learn more about glaucoma and how you can be tested for this serious condition, please call us today to schedule an appointment with one of our doctors.
Glaucoma Surgery
When eye drops do not adequately lower eye pressure enough to control a patient’s glaucoma, laser surgery or other glaucoma surgery may be recommended. Patients with a special condition called narrow angles can have angle closure glaucoma attacks, which can be prevented or treated with laser surgery to the iris.

Common Surgeries Include:
- Laser Peripheral Iridotomy (LPI) – For patients with narrow-angle glaucoma. A small hole is made in the iris to increase the angle between the iris and cornea and encourage fluid drainage.
- Argon Laser Trabeculoplasty (ALT) and Selective Laser Trabeculoplasty (SLT) – For patients with primary open angle glaucoma (POAG). The trabecular passages are opened to increase fluid drainage. ALT is effective in about 75% of patients, and SLT may be repeated.
- Nd: YAG Laser Cyclophotocoagulation (YAG CP) – For patients with severe glaucoma damage who have not been helped with other surgeries. The ciliary body that produces intraocular fluid is destroyed.
- Minimally Invasive Glaucoma Surgery (MIGS): For patients with mild to moderate glaucoma and certain MIGS can be performed in conjunction with cataract surgery.
- Filtering Microsurgery (Trabeculectomy) – For patients who have not been helped with laser surgery or medications. A new drainage passage is created by cutting a small hole in the sclera (the white part of the eye) and creating a collection pouch between the sclera and conjunctiva (the outer covering of the eye).
- Tube Shunt Surgery – May be recommended for patients with neovascular glaucoma, failed trabeculectomy, or susceptibility to developing scar tissue. A thin, flexible tube (a shunt) with a silicone pouch is inserted in the eye to facilitate drainage.


